Last Updated on 2 years by Publishing Team
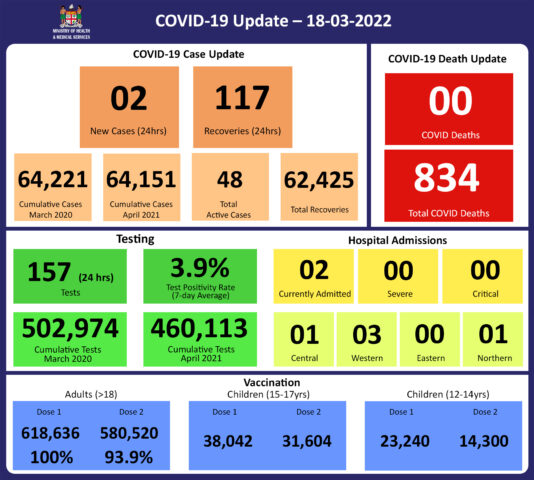
COVID-19 Update
Friday 18th March
Public Advisory:
COVID-19 Vaccination
As of 18th March, a total of 113,453 individuals have so far received booster doses. Members of the public are advised to obtain their booster dose after at least 5 months from their second COVID-19 vaccine dose. Moderna vaccine and Pfizer vaccines are both available for adult booster doses.
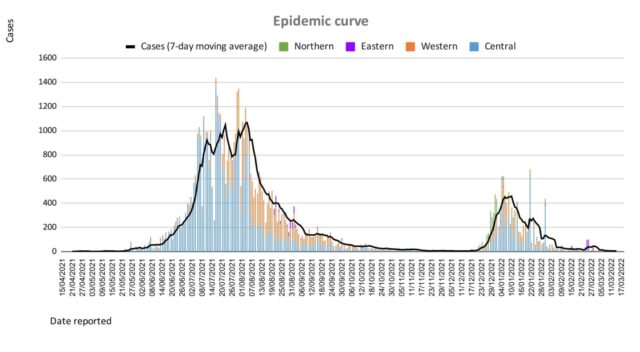
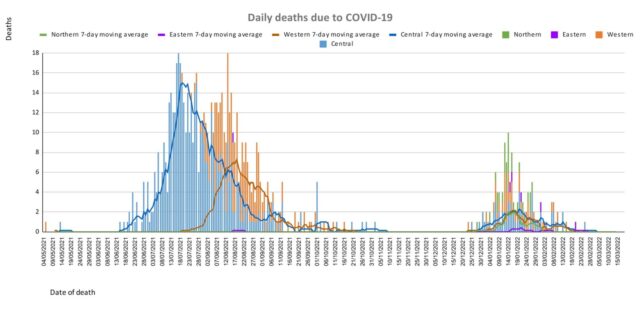
Our vaccination efforts in children are currently progressing well. While we have reported 100% first dose coverage for the adult population (i.e. people aged 18 and over), our coverage includes all adults living in Fiji at the time of our vaccination campaign, and we expect that there will be pockets of unvaccinated adult individuals. The two-dose vaccination coverage of our entire vaccine eligible population (all persons 12 years old and beyond) is 87% and we are extremely proud of our high vaccination coverage. The impact of our vaccination program and the high vaccination rate we achieved has been clearly demonstrated by the fact that case numbers and severe disease outcomes were significantly mitigated in the West during the second wave (Delta variant). Furthermore, the health impact of the last wave (Omicron) was mitigated by our collective engagement in the Vaccine Plus measures. Our borders were opened safely because of the high level of protection we built up together.
Our current booster program has been slowed down by slower uptake and deployment challenges relating to the need to deal with the current surge of leptospirosis, typhoid, dengue fever, and influenza we are facing Fiji-wide. The public is reminded to get booster vaccine doses, and the list of vaccination sites is provided daily on the MOH webpage. We expect decreasing immunity from the 2 doses of vaccines as well as decreasing post-infection acquired immunity over time. COVID is endemic in Fiji, as it is in most of the world, which basically means it is always present. We have opened international travel while Europe, China, New Zealand, and Australia are experiencing surges in COVID cases. Therefore, we reiterate that all eligible adults get a booster dose so we can reduce the risk of future surges of COVID-19 in terms of severe disease and hospitalisation, and avoid the institution of severe public health measures.
We will continue to monitor the evidence on post-infection immunity based on quality data that is being generated globally. However, until we have a better sense of the role of post-infection immunity, the Ministry of Health will continue to define our level of protection based on vaccination numbers
Given the current stocks of Pfizer vaccine we have, we will be using Pfizer for the ongoing primary 2 dose schedule of children and adults and as the booster dose.
Influenza
The current surge in influenza cases has added further strain to our outpatient care capacity, as we continue to see a high number of LTDD cases in our communities, while also continuing our efforts to support COVID-19 vaccination needs. These factors together only increase the pressure on all healthcare services, especially our outpatient facilities.
Before the pandemic, Fiji’s influenza season typically began in January and ended by May/June. However, in 2020 and 2021 there was a marked decrease in cases of influenza detected, a trend that was also seen in other countries. It is likely that public health and social measures deployed for COVID-19 worked to decrease other respiratory viruses, including influenza. The current increase in cases suggests a return to pre-pandemic levels of seasonal influenza, however, it is also possible that decreased incidence of influenza in recent years will have led to decreased immunity in the community, and subsequently more people becoming ill than in a usual flu season.
Children under the age of 5 (especially babies) and the elderly are most at risk of severe influenza, and we have published advisories on how to care for oneself and for children with flu, and the symptoms to watch out for especially as related to seeking extra care (https://www.health.gov.fj/influenza/).
The Ministry has been working on measures to open more facilities with extended service hours and to streamline outpatient services to help reduce waiting times. Many of our staff have returned from annual leave that had been deferred during the second and third waves of COVID-19, as well as sick leave during this increase in flu. We have also made adjustments in our outreach programs to deal with LTDD, and vaccination needs, in order to free up staff for outpatients services in health centers to help improve services. The Ministry is also pursuing the engagement of General Practitioners to provide outpatient services to the general public in a public-private partnership arrangement during this surge of Influenza infections.
Leptospirosis, Typhoid fever, and Dengue fever
The current wet weather around the country continues to promote the surge of leptospirosis, typhoid, and dengue fever in all divisions in the country. Though we have noted a decrease in hospital admissions, we are also aware of continued heavy rain in parts of the country, particularly the Western Division, and surges of leptospirosis cases, hospitalizations, and deaths following such weather events. As such the medical advice we provide needs to be followed, while we continue to mount our public health and clinical response. Please heed our advice to protect yourselves and your loved ones.
Leptospirosis
There have been 1230 lab-confirmed cases of leptospirosis this year, with 240 new cases to report since the last update a week ago, with 145 cases in the last week, and 94 more recorded for previous weeks. Outbreaks are ongoing in all four divisions.
In the Central Division, there have been 436 cases, with 100 in the last week and 77 more cases for previous weeks.
In the Western Division, there have been 488 cases, with 42 new cases in the last week, and 56 more reported for previous weeks.
In the Northern Division, there have been 270 cases, with 7 in the last week, and 9 more reported for previous weeks.
In the Eastern Division, there have been 36 cases, with 5 in the last week, and 7 more reported for previous weeks.
For national leptospirosis hospital admissions so far this year, there have been 380 people admitted in total. There have been:
* 206 admissions in the West, with 32 new admissions last week, and 38 in the previous week, indicating a downward trend in admissions. The most admissions last week were in Lautoka hospital, and Rakiraki, followed by Nadroga/Navosa and Nadi, Ba, and Tavua. A downward trend of admissions is noted in all subdivisions.
* 122 admissions in Central with 6 admissions last week, and 20 in the previous week, indicating a continued downward trend.
- * 40 admissions in the Northern Division, with 3 new admissions last week, and 10 in the previous week, indicating a downward trend
* 12 admissions in the Eastern Division, with 2 in the last week, and 6 in the previous week, indicating a downward trend. The admissions in the Eastern Division have been from Levuka, Kadavu, and Lomaloma.
Sadly, there are 2 more deaths caused by leptospirosis to report since the last update on 09/03/22: a 27-year-old who died in the Lautoka Hospital ICU on March 10th, and a 27-year-old in Wainibokasi on March 2nd. There have been a total of 27 deaths from leptospirosis this year, with 19in the Western Division, 3 in Central, and 5 in the North.
While we have seen cases in all age groups. Cases remain predominantly in the 10-39-year-old age group, with more in males than females, and in people of i-Taukei ethnicity.
Prevention
The leptospirosis bacteria is spread to humans through the urine of infected animals, such as cows, pigs, rats, and dogs. To reduce your individual risk, it is important to understand that exposure to animals, soil, mud, and floodwaters during work or recreational activities increases your risk of infection.
Important prevention measures include wearing full covered footwear at all times when going outdoors, avoiding wading or swimming in flooded waters, using clean fresh water to wash up after exposure to muddy waters, and keeping all food and drinks covered and away from rats. For workplaces, practice good personal hygiene at all times, cover cuts and wounds well, and use protective equipment, especially footwear when in flooded and/or muddy areas.
We are also urging all parents and guardians to prevent children from playing in the mud or swimming in flooded rivers or creeks, and ensure that they wear shoes when outside.
Symptoms and treatment
Early treatment can decrease the severity and duration of the disease. Please seek medical care if you have recently had contact with floodwaters, mud, or animals, and develop the following symptoms: fever, muscle pain, headache. You may also have red eyes, loss of appetite, nausea/vomiting, dizziness, or feel weak.
Leptospirosis can be treated with appropriate antibiotic medications prescribed by a doctor if treatment is sought early. Danger signs for severe leptospirosis include shortness of breath, coughing blood, chest pain, yellow eyes/skin (jaundice), signs of bleeding (including unexplained bruising), decreased or increased urination, difficulty staying awake. Severe leptospirosis is life-threatening, and anyone with these symptoms must be taken to the hospital immediately.
The reports from the recent FEMAT outbreak response visits to the Navosa Subdivision and the Ra Subdivision have shown that when patients are seen early and the appropriate treatment is provided, the patients were able to be treated successfully at home and not require admissions into the hospital. The number of severe diseases and deaths were all significantly reduced. So we encourage those who are sick at home to seek treatment early so they can recover quickly from their illness.
Typhoid fever
There have been 67 lab-confirmed cases of typhoid fever this year, with 15 in the last week (10 from the Western Division and 2 each from Northern and Central Divisions). Nationally, and in the Central, Northern, and Eastern Divisions, typhoid cases are below the average, or at the average numbers expected for this time of the year. However, in the Western Division, there are localized outbreaks in communities in Ra, Lautoka, and Nadi. Sadly, there have been 5 deaths from typhoid fever this year. There have been no new deaths reported since the last update on 9/03/22.
Typhoid fever is typically found in areas that do not have access to proper toilet facilities and/or clean drinking water. We strongly encourage people who live in rural areas, informal urban areas, and any other areas where access to clean drinking water is limited, to boil all drinking water. We must all also continue to practice basic hygiene measures such as frequently washing hands with soap and water, especially after visiting the toilet and before eating or preparing food.
The preliminary reports from our WASH projects in the Northern division have shown that when communities focus on ensuring good water supply, practising proper hand hygiene, have proper human waste disposal (hygienic toilet facilities), and with complete treatment of those with the disease, the outbreak of typhoid can be stopped in the community. So we encourage all our communities to focus on clean and hygienic WASH facilities to stop the spread of Typhoid fever in the community.
Dengue fever
There have been 1085 lab-confirmed cases of dengue fever so far this year, with 120 new cases since the last update. There are outbreaks in the Western Division (Nadi, Tavua, Ba), however, the decreasing number of suspected dengue cases presenting to health centers in the West is indicating a downward trend.
We continue to urge everyone to get rid of potential mosquito breeding places, such as empty containers inside and outside your homes that may collect water, including discarded tires, flower vases, and pot plant bases. Protect yourself from being bitten by mosquitoes by using mosquito screens in your homes, and mosquito repellents.